
Opioid addiction is a chronic disorder where individuals become physically and psychologically dependent on opioid medications. It often develops after prolonged use of prescription painkillers or illicit drugs, leading to altered brain chemistry and compulsive drug-seeking behavior.
The dangers of opioid addiction lie in its potential for overdose, severe health complications, and death. The CDC reported an estimated 81,083 opioid overdose deaths in the US during 2023.
In this article, we will scour the risks linked with poorly managed opioid addiction treatment and discuss strategies for safe, effective recovery approaches.
The Role of Prescription Medications in Opioid Treatment
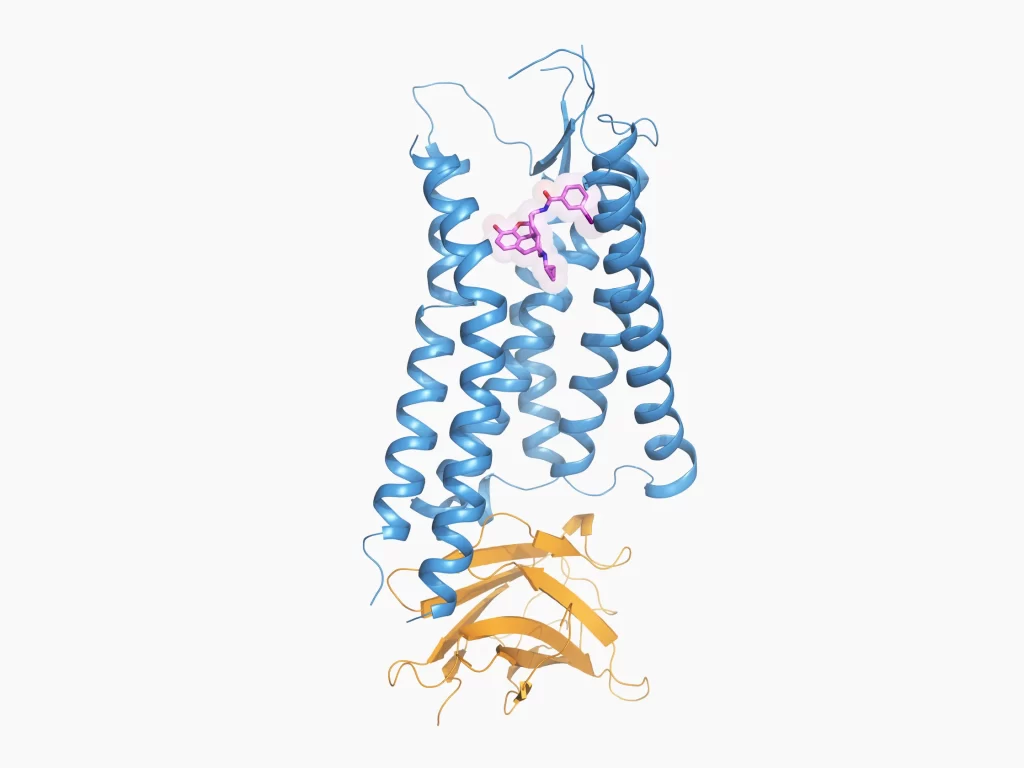
Prescription medications play a crucial role in opioid addiction treatment, particularly in easing withdrawal signs, reducing urges, and preventing reversion.
The National Institute on Drug Abuse reported that out of all opioid addicts, only 22% can get proper medication. However, medications such as methadone, buprenorphine, and naltrexone are highly effective in stabilizing patients, but they are not the only solution. A more comprehensive treatment is required for effective results.
Comprehensive therapy often includes behavioral therapy, counseling, and aid systems to address the psychological and social aspects of addiction. Prescription medication is important because it helps balance brain chemistry, allowing people to focus on healing without the overwhelming urge for opioids. However, a holistic approach combining medication with therapy offers the best chance for long-term success.
Risks of Over-Prescription

Over-prescription refers to the practice of prescribing medications, especially opioids, in amounts or frequencies that exceed the patient’s actual medical needs. This can lead to serious risks, including dependency, addiction, and overdose. Patients may generate a tolerance, requiring loftier doses for the same result, increasing the possibility of misuse.
According to the American Psychiatry Association, around 3% to 19% of persons taking prescription medications might develop a strong addiction. They may also switch to heroin for pain relief, which is more readily available. Over-prescription also contributes to the availability of opioids for non-medical use, fueling the opioid crisis.
Other risks include adverse drug interactions, side effects, and prolonged health complications. Addressing over-prescription requires stricter guidelines, monitoring, and instruction to ensure that medicines are used safely and efficiently.
How can overprescribing lead to increased dependency on medications?
Overprescribing can lead to increased dependency as patients may develop a tolerance, requiring more elevated doses to achieve the identical effect. This escalates the risk of addiction, as frequent and prolonged use of medications like opioids alters brain chemistry. All this makes it harder to stop without experiencing withdrawal symptoms.
Mismanagement of Treatment Plans
Mismanagement of treatment plans occurs when opioid addiction treatment is poorly coordinated or improperly monitored. This can happen due to inadequate patient assessments, lack of individualized care, or inconsistent follow-up. Healthcare providers, treatment centers, and patients share responsibility for ensuring proper management.
Physicians may fail to adjust medications or ignore signs of relapse, while patients may not adhere to prescribed plans. Correcting this requires regular communication between healthcare professionals and patients. Also, comprehensive treatment, including medical and psychological support and ongoing monitoring to adjust care as needed, ensures the treatment is both effective and safe.
How can patients advocate for personalized treatment plans with their healthcare providers?
Patients can advocate for personalized treatment plans by openly discussing their specific needs, health concerns, and therapy objectives with healthcare providers. They should ask questions, request alternative options if essential, and energetically participate in decision-making. It will ensure the plan addresses both their physical and mental health in addiction recovery.
Side Effects of Prescription Medications
Prescription medications used in opioid dependence treatment can cause diverse side effects, varying from mild to intense. Common issues include nausea, dizziness, fatigue, and mood changes. For instance, methadone may lead to respiratory problems, while buprenorphine can cause liver complications.
According to Trulaw, Suboxone, a combination of buprenorphine and naloxone, is linked to significant dental health problems, including tooth decay, cavities, and oral infections. These issues emerged as patients experienced severe tooth damage despite good dental hygiene. If someone has faced a similar issue, they are eligible for filing a lawsuit.
The adverse effects of Suboxone on oral health led to a series of lawsuits. In the Suboxone lawsuit, the plaintiffs are claiming the drug’s suppliers failed to sufficiently warn patients about these potential dangers and complications. They can claim compensation through these lawsuits.
How do side effects impact a patient’s recovery journey and quality of life?
Side effects can hinder a patient’s recovery journey by causing discomfort, discouraging treatment adherence, and potentially leading to additional health issues. These complications can lower life quality, making it harder for individuals to focus on long-term recovery while managing both physical and mental challenges.
Lack of Support and Monitoring
Lack of support and monitoring in opioid addiction treatment can significantly undermine a patient’s recovery. Without proper oversight, patients may struggle with adherence to treatment plans, miss signs of relapse, or fail to address emerging health complications. Inadequate support, such as limited access to counseling, peer groups, or follow-up care, leaves individuals vulnerable to setbacks and emotional distress.
A study by the National Library of Medicine revealed that as the dose of opioids gradually decreases, there is a decrease in overdose events. A considerable difference of 30-90% is seen if the opioid dose is reduced from 18 to 1.8. The only important actions here are monitoring and support.
Healthcare providers are responsible for regularly monitoring progress, adjusting treatments as necessary, and providing comprehensive support systems. Addressing these gaps through consistent communication, ongoing evaluation, and access to mental health services can enhance the effectiveness of addiction treatment and long-term recovery.
Stigmatization and Its Health Impact

Stigmatization surrounding opioid addiction can have profound negative effects on a person’s health and recovery journey. Those facing stigma often experience shame, isolation, and reluctance to seek help, delaying treatment and exacerbating their condition. Fear of critique from healthcare providers, bosses, or even loved ones can prevent individuals from openly discussing their struggles.
This stigma can lead to untreated mental health issues, increased substance misuse, and a higher risk of relapse. Addressing stigmatization requires public education, compassionate healthcare approaches, and support systems that prioritize empathy and understanding. It creates a safer atmosphere for people to seek help and recover without fear of discrimination.
Strategies for Safe and Effective Treatment
Safe and effective opioid addiction treatment requires a combination of medication, behavioral therapy, and ongoing support. Medications like buprenorphine or methadone help manage withdrawal signs and cravings, while cognitive-behavioral therapy (CBT) manages the psychological characteristics of addiction. Personalized treatment plans, regularly monitored by healthcare providers, ensure adjustments are made based on progress.
For example, integrating group therapy alongside medication can provide emotional support and accountability. Regular check-ins and holistic care, including mental health counseling and lifestyle adjustments, further promote recovery. These strategies work together to create a balanced approach, reducing relapse risk and improving long-term success in overcoming opioid addiction.
A Holistic Approach to Opioid Addiction Recovery
Addressing opioid addiction requires a well-rounded approach combining medical treatment, psychological support, and consistent monitoring. Safe and effective recovery is possible when healthcare providers offer personalized care while patients advocate for their needs. With the right strategies, individuals can retrieve control over their energies and overcome the challenges of opioid dependence.




